
The physicians and health care professionals in The GW Medical Faculty Associates Division of Endocrinology & Metabolism excel at providing comprehensive evaluation, diagnosis, treatment and management of endocrine disorders. These include diabetes, thyroid diseases, bone and mineral disorders, adrenal and pituitary diseases, endocrine tumors and reproductive disorders.
In addition to providing superior patient care, our physicians conduct clinical research in endocrine disorders and offer the most effective, advanced treatment options and technologies.
Overview of the Endocrine System
Hormones are small molecules that are released into the bloodstream by the glands of the endocrine system. Hormones include cortisol, thyroid hormones, insulin, testosterone, estrogen and many others. They act as messengers, delivering signals and commands that help to control growth and development, reproductive functions, metabolism, responses to stress, and electrolyte and fluid imbalance.
Our endocrinologists are skilled at recognizing the many different effects of hormones and at associating a patient’s symptoms with a specific hormone abnormality. Because endocrine dysfunction can have widespread effects, endocrine disorders are oftentimes best treated by a multi-specialty team. At The GW Medical Faculty Associates, endocrinologists work with cardiologists, surgeons, ophthalmologists, obstetricians, podiatrists, kidney doctors and many others in our multi-specialty practice to provide comprehensive management of complex endocrine disorders.
The endocrinology team encourages full patient participation in treatment decisions. We believe that clinical management should make sense to our patients and meet their individual needs and priorities.
Disorders of the Endocrine System
Endocrine disorders may involve production of too much or not enough of a specific hormone. For example, in hyperthyroidism, the thyroid gland releases too much thyroid hormone. In patients with type 1 diabetes, pancreatic beta cells have been damaged and do not produce any insulin.
Hormones act on most cells and tissues throughout the body. Therefore, patients with endocrine disorders have many different symptoms and clinical problems. A man with hyperthyroidism may experience a rapid heart rate; a women with a prolactin-secreting pituitary tumor may experience a halt in her menstrual periods or notice a breast discharge.
- Diabetes
-
Individuals with diabetes have an elevated blood glucose (sugar) level. Diabetes develops when the body does not produce enough insulin or when cells don’t respond properly to the insulin that is present. If blood sugar remains elevated for a long time, diabetes can lead to damage to the heart, blood vessels, eyes, kidneys and nerves.
The two most common forms of diabetes are type 2 diabetes and type 1 diabetes.
Type 2 Diabetes
Type 2 diabetes usually develops in people over the age of 40, although it is becoming increasingly common in younger adults and adolescents as well. About 90 to 95 percent of adults with diabetes have type 2 diabetes.
In people with type 2 diabetes, the pancreas may produce some insulin, but the body does not respond to the insulin effectively. This condition is known as insulin resistance. Obesity frequently contributes to insulin resistance.
The first step in treating diabetes is an appropriate diet and exercise program. At The GW Medical Faculty Associates, patients with diabetes meet with trained diabetes educators and dieticians to fashion individual plans that enable patients to maintain an appropriate weight, eat a healthy diet and exercise regularly.
If diet and exercise fail to keep the blood glucose in or near the normal range, oral medications may be prescribed. Some patients do not respond to oral medications and may require insulin or another injected medication.
Type 1 Diabetes
Type 1 diabetes develops most often in children and young adults. In patients with type 1 diabetes, the immune system mistakenly attacks the insulin-producing beta cells in the pancreas and destroys them. The pancreas then produces little or no insulin. People with type 1 diabetes always require insulin.
Diabetes Treatment
Managing diabetes can seem overwhelming. At The GW Medical Faculty Associates, our multi-disciplinary clinical and educational services team helps make life easier—and safer—for our patients with diabetes.
In addition to ongoing evaluation and medical care, counseling and support are part of the treatment plan for all of our diabetes patients. We provide diabetes education, diabetic foot care and nutritional counseling.
Our certified diabetes educator develops individually- tailored diet and exercise plans, and teaches our patients the skills they need to confidently manage their diabetes.
Insulin therapy
Insulin cannot be taken orally; it must be injected. Many patients are anxious when told that they must start taking insulin. Modern, small needles and self-contained “pen” devices make administering insulin easier than patients expect.
Patients on intensive insulin programs—taking multiple injections of insulin and frequently adjusting their insulin doses—may benefit from some of the new technologies that are now available. Insulin pump therapy, continuous glucose monitoring and computer display systems allow patients to carefully monitor and manage their blood glucose levels. Our staff can help patients master the newest technologies available for diabetes care.

Suzanne Adler, M.D., Associate Clinical Professor of Medicine Diabetes and pregnancy
Pregnancy poses special challenges for women with diabetes. A healthy pregnancy requires vigilant blood sugar control from conception onward.
Ideally, women with diabetes who are planning to become pregnant should schedule a thorough evaluation by an endocrinologist before conception. Careful planning and treatment adjustments can reduce or avoid many of the risks that diabetes can pose to mother and baby.
At The GW Medical Faculty Associates, the endocrinologist, diabetes educator and dietician work with obstetricians to provide support to women with diabetes who are pregnant. Frequent monitoring contributes to a healthy pregnancy and a healthy baby.
Gestational diabetes
Sometimes diabetes develops during pregnancy. If untreated, gestational diabetes may lead to problems for the mother and the baby. Complications include high blood pressure for the mother and abnormally large size for the baby; both can lead to risks during delivery. If blood sugar is not well controlled, the baby can be born prematurely. Because women with gestational diabetes generally have no symptoms, most obstetricians screen women for diabetes during pregnancy.
Gestational diabetes can usually be managed with diet and exercise. If diet and exercise modifications are insufficient, then medication, including insulin, may be required.
Gestational diabetes generally resolves at delivery. However, it is a warning sign that the woman is at increased risk to develop type 2 diabetes later in life. Post-delivery, our endocrinologists continue to see patients who have had gestational diabetes, in part to develop and encourage a sensible diet and exercise plan that will keep them healthy.
- Thyroid Conditions
-
Thyroid hormones regulate many aspects of cell and organ function, including energy metabolism and brain development and function. The GW Medical Faculty Associates endocrinologists evaluate, monitor and treat all thyroid disorders.

Hyperthyroidism and Hypothyroidism
When the thyroid doesn’t produce enough hormone, the diagnosis is hypothyroidism; if too much hormone is produced, the result is hyperthyroidism.
Unexplained fatigue and/or weight gain are common symptoms of hypothyroidism. Other effects of this condition can include high cholesterol and depression. Symptoms of hyperthyroidism include unexplained weight loss, racing heart rate, anxiety and sleep problems.
Hypothyroidism is treated by thyroid hormone replacement. The prescription medication levothyroxine is biochemically identical to the major thyroid hormone made by your own thyroid gland. Using sensitive biochemical tests, our endocrinologists can exactly match your thyroid replacement dose to your individual requirement.
There are several options for treatment of hyperthyroidism including medications, radioactive iodine and surgery. There are advantages and disadvantages to each. At The GW Medical Faculty Associates, thorough discussions between endocrinologist and patient determine the choice of treatment, balancing patient priorities and concerns with the physician’s recommendation.
Goiter, Thyroid Nodules and Thyroid Cancer
Goiter refers to an enlarged thyroid gland. There are many different causes of goiter and not all of them require treatment. Thyroid nodules or goiter may be found by the patient or may be discovered during a routine physical examination.
We use a number of techniques to evaluate goiter and nodules. Blood tests can help to determine if a goiter or nodule is causing hyperthyroidism. Imaging studies, including thyroid ultrasonography and the nuclear thyroid scan, can further characterize a nodule. Fine needle aspiration is done to obtain a small sample of thyroid cells for analysis.
Although most goiters and thyroid nodules are benign, about five to ten percent are malignant. Long-term outcomes for the most common forms of thyroid cancer are excellent. We refer patients to highly experienced thyroid surgeons for removal of these tumors. Following surgery, scans and imaging procedures may be required; some patients need radioactive iodine treatment. Thyroid hormone replacement is initiated after surgery and closely monitored thereafter.
- Reproductive Disorders
-

Michael Irwig, M.D., F.A.C.E, Associate Professor of Medicine Endocrinology and Reproduction
Our endocrinologists are often part of a team of The GW Medical Faculty Associates physicians providing the most current and creative strategies to help couples with infertility issues that include absent or irregular menstrual cycles, abnormal sperm production, failure to conceive or frequent miscarriages in early pregnancy. We also monitor and treat medical conditions such as diabetes and thyroid disorders during pregnancy.
Polycystic Ovary Syndrome and Increased Androgens
Women who have irregular or absent menses along with facial hair growth or acne may have polycystic ovary syndrome (PCOS), which also can cause difficulty in conceiving.
The treatment of PCOS should be individualized to match the woman’s primary concerns. An oral contraceptive may be appropriate to regulate periods in a woman who is not trying to become pregnant. However, if the woman is trying to conceive, we have alternative medications and approaches. In some women, PCOS is associated with an increased risk of type 2 diabetes; sometimes we prescribe metformin, a medication commonly used to treat diabetes, to treat PCOS.
Androgen Deficiency
Sexual dysfunction in men (low sex drive, erectile dysfunction, infertility and lack of spontaneous erections) and non-sexual problems such as low energy, depressed mood and sleeping problems may be due to a low testosterone level. Testosterone deficiency may be the result of an endocrine disorder involving the testes or pituitary, an underlying medical disorder or medications such as narcotics or steroids.
We diagnose low testosterone by measuring testosterone and other hormone levels. We can treat androgen deficiency with testosterone that is delivered by topical gels, patches or injections. Regular follow-up visits are recommended to monitor the dosage.
- Calcium Disorders and Osteoporosis
-
Hypercalcemia
If the calcium concentration in the blood is too high (hypercalcemia), it can interfere with nerve and brain function and can damage the kidney or lead to weakened bones. Many patients have asymptomatic hypercalcemia that is discovered by a routine blood test. The most common cause of hypercalcemia is hyperparathyroidism, overactivity of the parathyroid glands. Most often this is due to the presence of a benign parathyroid tumor. Using sensitive blood tests, nuclear scans and ultrasonography, our endocrinologists locate these tumors and refer patients for curative surgery.
Osteoporosis
Our bones are made up of calcium, collagen, minerals and living cells. Vitamin D and parathyroid hormone work together with other hormones to control the calcium in our bones. For healthy bones, it is important to maintain appropriate calcium intake and vitamin D levels. In addition, regular exercise can help to maintain bone strength and reduce the risk of falls that could result in broken bones. Low bone density is treated with medication when necessary.
Bones are constantly regenerating; old bone is replaced by new. Osteoporosis results when there is an imbalance between the resorption of old bone and the production of new bone. Osteoporosis does not cause symptoms until a bone breaks. Therefore, individuals, especially those at high risk, need to be screened. All women age 65 and over and men age 70 and over should be screened for osteoporosis with a DEXA scan. Earlier testing is indicated for individuals at high risk due to early menopause, rheumatoid arthritis, long-term steroid treatment or previous low-impact fracture.
- Pituitary Disorders
-
The pituitary gland is sometimes called the “master gland” because it produces several different hormones that control the thyroid gland, the adrenal glands, the testes and the ovaries. The pituitary is also involved in the control of growth in children and in the regulation of thirst and water balance. The pituitary gland contains several different types of cells; each is specialized to control a separate pituitary function.
Pituitary tumors
Pituitary adenomas are benign tumors of the anterior pituitary that may produce excess hormones. Symptoms of pituitary adenomas depend on the type of pituitary cell in the tumor. Since the optic nerve runs close to the pituitary, a very large pituitary tumor can affect vision. At The GW Medical Faculty Associates, endocrinologists closely collaborate with neurosurgeons, neuro-ophthalmologists and other specialists in the treatment of pituitary tumors.
Cushing’s disease results from a pituitary adenoma that secretes the hormone ACTH, which directs the adrenal glands to overproduce cortisol, the stress hormone.
Symptoms of Cushing’s disease include unexplained weight gain, increases in blood sugar and blood pressure, unexplained bruising and profound decreases in energy. Surgery is typically required for the initial management of Cushing’s disease.
Acromegaly results from a pituitary tumor secreting excess growth hormone. Symptoms include increases in ring size, shoe size, tongue size and jaw prominence. We treat acromegaly with a combination of surgery and medication.
Prolactinomas are benign tumors that produce the hormone prolactin, which normally controls milk production in nursing mothers. Prolactinomas in women may be the cause of menstrual irregularities and milky secretions from the breasts. For men, a prolactinoma may decrease their, testosterone level, libido and fertility. Most prolactinomas can be treated with medication and do not require surgery.
We diagnose pituitary adenomas with blood tests to measure anterior pituitary hormones and an MRI to image the pituitary gland. Following initial surgery for a pituitary tumor, follow-up is generally required to assess post- operative pituitary function and to determine if additional treatment is required.
- Adrenal Gland Conditions
-
Cortisol is a steroid hormone produced by the adrenal gland that prepares the body to respond to stress. Cushing’s syndrome and Addison’s disease (adrenal insufficiency) are conditions of too much and not enough cortisol production, respectively. Symptoms of Cushing’s syndrome include fatigue, mood swings, reddened and rounded face, easy bruising and muscle loss. There are several different causes of Cushing’s syndrome and the endocrinologist must investigate carefully to determine the correct diagnosis.
The adrenal glands also produce hormones (catecholamines and aldosterone) that help to regulate blood pressure. Usually, hypertension, or high blood pressure, is best treated with medications. However, occasionally hypertension can be the result of an adrenal tumor producing catecholamines (pheochromocytoma) or aldosterone. In those cases, surgery may cure or substantially improve the hypertension.
Division of Endocrinology
The GW Medical Faculty Associates Division of Endocrinology & Metabolism is affiliated with The George Washington University School of Medicine & Health Sciences, an academic hospital with the most recently developed medical technology in use today.
3rd Floor
22nd St NW & I St NW
Washington, DC 20037
Parking
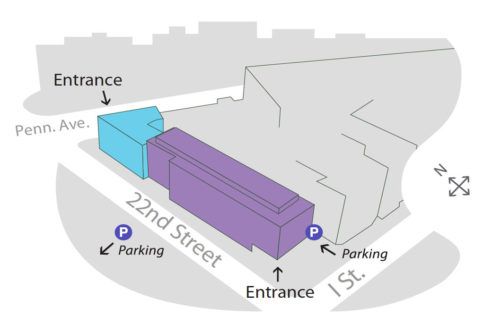
The Division of Endocrinology is located at 22nd & I Streets, NW. Garage parking is available either just east of our circular drive at 22nd & I Streets or on 22nd Street midway between I Street and Pennsylvania Avenue. The MFA is one block east of the Foggy Bottom Metro Station (Orange & Blue Lines).
